Blog # 9 - Kidney Supportive Care in Brisbane, Metro North Health.
My next clinical placement in Australia was in Brisbane, where I was based at the Royal Brisbane and Women’s Hospital (RBWH). I also attended and spoke at the annual Australian KSC Masterclass.
Speaking at the annual Australian Kidney Supportive Care Masterclass
This blog will cover the following:
Development of a kidney supportive care service for Brisbane, Metro North Healthcare
Components of the kidney supportive care team
Australian National Palliative Care Standards
My first experience of voluntary assisted dying
Australian Kidney Supportive Care Masterclass
Metro North Health Network:
Metro North Health network operates the Royal Brisbane and Women’s Hospital (RBWH), several other hospitals and community health centres from north of the Brisbane River to north of the town of Kilcoy and serves a population of 900,000. Brisbane and Women’s Hospital (RBWH) is the largest hospital in Australia, the biggest teaching and research hospital in Queensland and has 929 beds. During my stay in Brisbane I spent time observing KSC clinics, time in the hospital renal unit and attended the annual Australian Kidney Supportive Care Masterclass where I also gave a talk.
On the KittyCat cross river transport, on the River Brisbane
Renal Service for Metro North Health:
The main hub for renal services is based at RBWH. Clinics are also provided at other hospitals or community health centres operated by Metro North Health, there is a satellite dialysis unit at North Lakes Health Precinct and hospital consultations are provided at RBWH and Prince Charles Hospital, where services include cardiothoracic surgery and transplantation. 65% of patients live within a 9 mile radius of RBWH Brisbane, so a significant proportion of the clinicians’ work is providing outreach services across Metro North Health either by face-to face consultations or by telehealth. This is a multi-cultural society where there is a high indigenous population. There is a large emphasis on delivering Aboriginal and Torres Strait Islander health services that are culturally appropriate and culturally safe as there is often a mistrust of healthcare professionals within this population.
Development of the Kidney Supportive Care service for Metro North Health:
As with many of the KSC services that I have visited, funding from the healthcare service was not available and so temporary funding was gained to start the service. In 2016, the Palliative Care lead for the RBWH, Dr Carol Douglas and one of the renal nurse consultants who provided renal-patient education, Ilse Berquier, successfully gained temporary funding through the SEED Innovation Fund, to develop a KSC service. The grant application was based on the increased numbers of people developing CKD, the evidence that patients with CKD have significant palliative needs and the knowledge that conservative kidney management may be a better treatment option for some frail, elderly patients than treatment with dialysis.
The staffing requested in the fund included a renal consultant (2 sessions), a palliative care consultant (2 sessions), a clinical nurse consultant (6 sessions), a social worker (2 sessions), a pharmacist and an admin officer. The aim of the service was to meet the palliative care needs of kidney patients in the hospital and community settings, provide dedicated conservative management clinics, provide support for treatment decision making, support for care around dialysis withdrawal, improve advance care planning and improve end of life care. One of the other goals was to improve the palliative care skills of the renal team. Evaluation was done by measuring Patient outcome measures (PROMS) which included symptoms (using the IPOS-renal), quality of life, patient and clinician satisfaction. An estimate of released value was also measured which included capacity freed in general nephrology clinics, reduced waiting lists for clinics, cost of avoiding dialysis, reduced avoidable admissions and shorter length of hospital stay.
The outcomes of the temporary service were positive and Metro Health North agreed to commit to permanent funding of the KSC team. However, demand on the service grew quickly. It is estimated that 10% of the population of Queensland have chronic kidney disease and in 2019, Queensland developed a state-wide policy ‘Advancing Kidney Care 2026’ which made improving healthcare for people with kidney failure one of the key priorities.
After multiple hospital executive meetings, presentations, education sessions and development of a business case from the Palliative Care Consultant Lead (Carol Douglas), the Renal Consultant Lead (Helen Healy) and the Renal Nurse (Ilse Berquier), Advancing Kidney Care 2026 funding was obtained and it was agreed to expand the service. This allowed a renal consultant to have more dedicated KSC sessions and a nurse practitioner role to be developed. Nurse practitioners in Australia are able to prescribe. The components of the current service are described below.
Components of the Royal Brisbane and Women’s Hospital Kidney Supportive Care service:
Medical support:
Renal Consultant – Dr Kirsten Hepburn (renal consultant with a Clinical Palliative Care Diploma) has 4 sessions per week dedicated to KSC. She provides 7 clinics per month and within these clinics she will see any renal patient requiring supportive care – those on dialysis, those receiving CKM, patients with advancing kidney disease making treatment decisions (including transplant patients).
She also sees patients who are known to the KSC service or who have supportive care needs if they are admitted to RBW Hospital or Prince Charles Hospital if the KSC nurses require consultant input. She also provides routine renal care in general nephrology clinics, the dialysis unit and within the acute hospital alongside 13 other consultant nephrologists.
Palliative Care Consultant – the hospital funds 4 sessions per week for palliative care consultants to provide KSC in the clinic setting and in the acute hospital setting. This is currently split between two of the hospital palliative care consultants. I spent time in clinic with Dr Katrina Kramer who is a palliative care consultant with a background in general practice. They provide the same role in the KSC clinic as the renal KSC consultant, and share discussion and care of patients if complexity means this is required.
Dr Katrina Kramer (Pall Care consultant), myself and Dr Kirsten Hepburn (Renal consultant) in a KSC clinic
KSC Nurse support:
The KSC service has 3 dedicated nurse specialists. Laura Austin, Clinical Nurse Consultant (4 days) who has recently completed a post-graduate certificate in Palliative Care, Ilse Berquier, Nurse Practitioner (3 days) and Catriona Bisset, Clinical Nurse (2.5 days). The nurses review any patient with KSC needs admitted to the acute hospital and receive input from Kirsten or the Palliative Care team if required. An alert system on the hospital’s electronic system will inform the KSC team if a patient known to the service is admitted to hospital. The nurses are also present at the KSC clinics with Kirsten or the Palliative Care consultants and can follow the patients up afterwards. They provide renal patient education, home-visits and outreach via telephone and telehealth as well as hospital consultations.
Social Work:
There is dedicated time for 2 days per week for a SW to provide support for KSC patients which includes attendance at clinic and MDT.
Pharmacist:
There is dedicated time for the KSC service from the renal pharmacist.
Admin
The KSC service has a full-time administrator. Her role includes phoning patients to arrange appointments (during which she often gathers useful personal information), setting up telehealth appointments, providing the patients with the PROM tools when they arrive at clinic and ensuring they are able to complete them. She supports the nurses with uploading the results of the PROMs and ACP onto the patient’s Electronic Health Record and the KSC data-base.
MDT meetings:
MDT discussions occur with the team before or after a clinic where there is a discussion about the patients who are seen that day.
PROMS and ACP
At every consultation the following tools are collected and documented electronically on the patient - an IPOS-renal, the EQ-5H (Quality of Life score) and the Australian-modified Karnofsky’s Performance Scale, is collected for the patient.
The patient electronic health record has a section on Advance Care Planning (ACP) and this is updated during consultations. The ACP in Queensland is legally binding and when a patient loses capacity, the person who has Power of Attorney has the right to make decisions regarding treatments such as dialysis and CPR on the patient. A member of the ‘Justice of the Peace’ (UK equivalent would be a registrar or lawyer) is required to overturn any decisions. This can sometimes lead to difficulties and so the KSC team often prefer to complete an electronic treatment escalation plan with the patient called the Statement of Choices which is not legally binding, but takes into account the patient’s values and wishes if they lose capacity. It is a similar document to the ReSPECT electronic tool which is being implemented across Scotland.
KSC Resources:
The team have developed a number of patient-information leaflets, educational resources, referral forms, a KSC patient-plan, KSC - patient data collection form and other documents. These are helpful for patient information, for staff education and for data collection and analysis.
KSC education:
As well as providing training for trainee doctors in renal and palliative care, the team organise an annual KSC symposium to educate on symptom control and other aspects of KSC. This was replaced in 2024 with the Australian KSC Masterclass which was held in Brisbane this year. The team also plan to start developing Fellowships in Kidney Supportive Care for renal and palliative care trainees.
Laura Austin, myself, Dr Katrina Kramer, Ilse Berquier, Catriona Bisset, Dr Kirsten Hepburn - the KSC core medical and nursing team
In my last blog, I shared the main points of the proposal to develop a Tasmanian-wide Kidney Supportive Care service and described the components required to deliver such a service. In Brisbane, over a few years which has involved gaining temporary funding, proving positive outcomes, persistence to engage with professionals at executive level and the case for a KSC service being listened to at executive level, Brisbane Metro North now has many of these components and provides a well developed, patient-centred KSC service.
Dr Kirsten Hepburn – Renal Lead for Kidney Supportive Care
Dr Kirsten Hepburn is the renal consultant who organised my sabbatical placement in Brisbane and the person I spent most time with in clinics.
Kirsten did most of her renal training in Sydney at St George Hospital which has a well-established and internationally renowned KSC service. This service has an integrated model with both renal and palliative care specialists who have dedicated time for KSC. At St George Hospital it is mandatory that all renal trainees attend KSC clinics and MDT meetings, therefore Kirsten had regular training in KSC as a registrar. She came to Royal Brisbane and Women’s Hospital to complete her training in 2019 at the time that the AKC 2026 funding for KSC had become available. In 2020 she started as a consultant nephrologist with 4 sessions of KSC in her job plan. In 2021, she was supported to do a 6 month Clinical Diploma in Palliative Care which involved her working with the Palliative Care team and developing her specialist skills. Kirsten now provides the medical leadership for the KSC service.
She is currently the acting co-chair of the Australian and New Zealand Society of Nephrology (ANZSN) Kidney Supportive Care specialist interest group (SIG).
Dr Kirsten Hepburn opening the annual Australian KSC Masterclass in Brisbane
Palliative Care Standards
One policy which has been helpful in making the case for resource to provide better palliative and supportive care models (for cancer and non-cancer) in healthcare is the Australian National Palliative Care Standards. This is a guide to best practice palliative care in different settings and works on the premise that delivery of palliative care is relevant to all healthcare professionals. Therefore, two sets of standards have been produced – one for Specialist Palliative Care and the other for All Health Professionals and Aged Care services. These standards are within the KSC Portfolio for Metro North Health so that the clinical work they provide, is based on the National Standards. Data collected about the service can be analysed and measured against the standards and service planned around the results
National Palliative Care standards for Providers of Palliative Care in Australia - 2024
Challenges:
Although this was one of the most integrated and comprehensive KSC services I visited on my sabbatical, there are still challenges which the service face. These have included having no social worker for 9 months, inequitable Allied Health Professionals access across sites, limited access to Psychology, challenges with succession planning and with recruitment to backfill leave. There is also a struggle to balance clinical demands with strategic, operational and research time. The latter is common to many clinicians in the NHS. Clinical work takes priority and demand is increasing, however, if we are unable to dedicate time for strategic and operational planning and for research, it is difficult to develop a service, prove effectiveness and share best practice.
Voluntary Assisted Dying:
Queensland legalised voluntary assisted dying (VAD) in 2021. This was interesting for me as I was in Brisbane 2 weeks before the Assisted Dying Bill was passed for England and Wales. During my time observing in clinic, a patient attended who had advanced kidney disease and was looking at treatment decisions. She was clear that she would not wish dialysis, but she was also clear that as she became more frail she would wish to receive VAD. She still had a good performance status but was very clear on her decision. Legally in Queensland, if a patient mentions VAD, the doctor must signpost the patient to VAD services (even just by mentioning that they can look them up online) and they also have to highlight the role of palliative care in relieving suffering. Kirsten handled the situation very professionally. Interestingly, in Queensland several dialysis patients have chosen VAD, despite the fact that they have access to good supportive care and withdrawal of dialysis can often allow a planned, peaceful death for patients. Anecdotally Kirsten feels that those dialysis patients who choose VAD do so as they wish an element of control over when and how they die and fear ‘lingering’ if they withdraw from dialysis.
Australian Masterclass for Kidney Supportive Care
Kirsten is currently Acting co-chair of the Australian New Zealand Society of Nephrology (ANZSN) Kidney Supportive Care specialist interest group. They meet regularly by virtual meetings throughout the year as well as organise an annual Masterclass. This is to promote teaching on aspects of KSC such as symptom control as well as share best practice or challenges in this area and network with other professionals interested in KSC.
The KSC Masterclass was held in Brisbane this year and I arranged my placement to coincide with this. It was organised by the KSC team, led by Laura Austin (Nurse Consultant). I was asked to speak at the Masterclass about the development of the NHS Tayside Renal Supportive Care model.
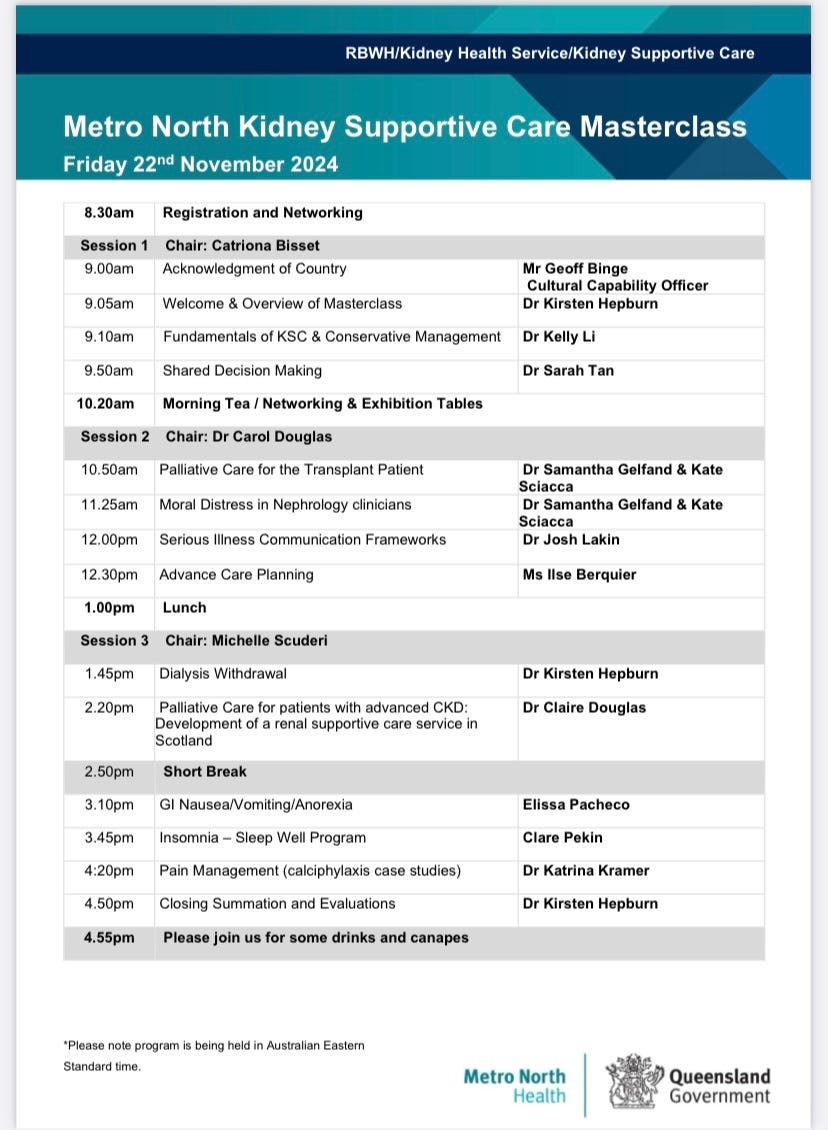
The KSC Masterclass programme
The programme was excellent and it was great to meet professionals interested in this area from across Australia, some of whom I spent time with on future placements. It was also fortuitous that the Renal-Palliative Care team from Boston Women’s Hospital were there. They had spent a week in Sydney at St George Hospital learning more from the KSC team and had also agreed to speak at the Masterclass. The team consists of Dr Samantha Gefland (consultant who is dual trained in renal and palliative care), Dr Josh Lakin (palliative care consultant), Kate Sciacca (KSC nurse) and Caroline Taverna (social worker). Sam has completed dual Fellowship training in renal and palliative care in the USA and spent time at St George Hospital, Sydney 6 years ago to further her interest in KSC. She has led the development of a service in Boston and now leads a multiprofessional team involving the colleagues who came to Brisbane. They gave a series of excellent, thought-provoking and informative talks.
The Boston Renal-Palliative Care team - Dr Samantha Gefland, Kate Sciacca, Dr Josh Lakin and Caroline Taverna.
Reflections from my Brisbane experience:
Brisbane has a very comprehensive KSC service and it was inspiring to see how the multiprofessional team work together to provide such an excellent integrated service which supports patients, carers and the wider renal team. The service is led by the renal department but also has funding to allow dedicated time from palliative care. This provides a good skill mix to allow joined-up, efficient and patient-centred care. Kirsten Hepburn, who provides the medical leadership from renal, has had training in renal, where KSC training was mandatory and also has a Clinical Diploma in Palliative Care. As a result, she is skilled in providing the clinical leadership, as well as providing strategic leadership and training for renal and palliative care trainees. The culture has changed within the overall nephrology team, so that KSC is considered as important as other aspects of kidney care. The KSC team have the skill and dedicated time to support colleagues in dealing with many of the palliative and supportive care needs of their kidney patients.
Clinical Diplomas in Palliative Care are not available in the UK. A diploma in Palliative Care is available, but this is more of an academic qualification than a practical and clinical experience.
In order to gain funding for the service initially, data collection and measurement of patient outcome was essential so that need, effectiveness and patient-centred care could be demonstrated, as well as showing that the service was economically valuable. However, to make the business case for the development of the service, having the Palliative Care lead and the Renal lead for RBWH hospital was probably also essential in order to have engagement at executive level